starting with results:
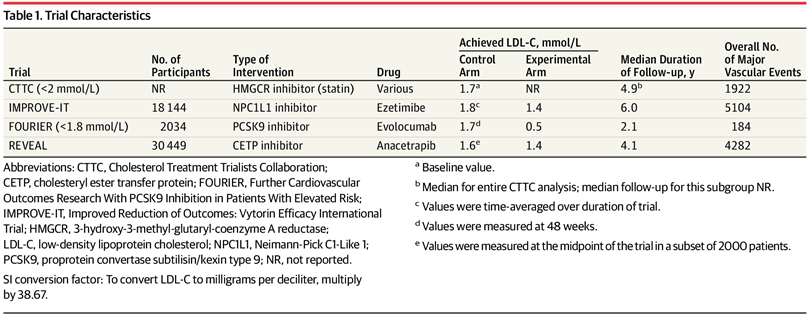
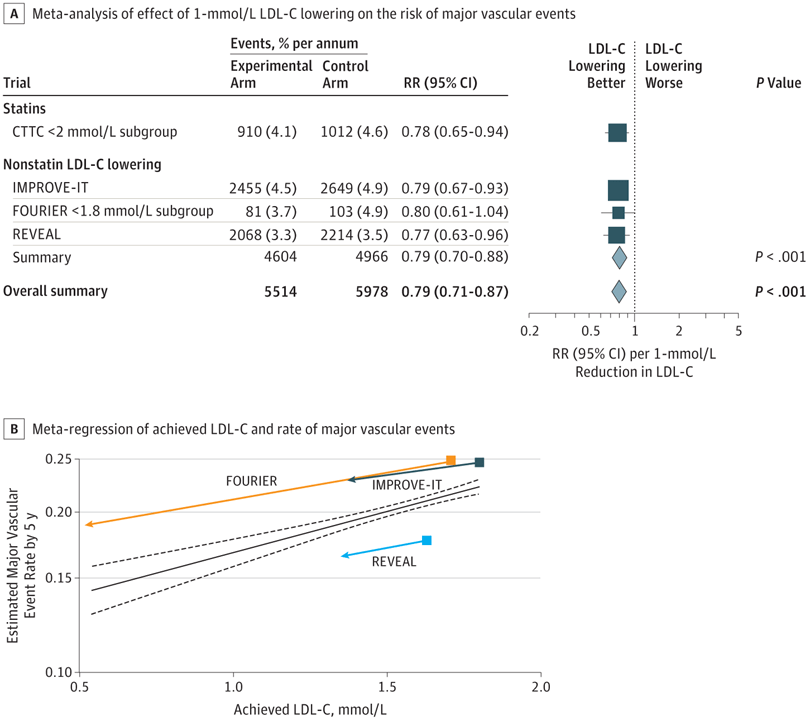
Nonstatin therapy lowered LDL-C by 11 mg/dL to 45 mg/dL, and the RR for major vascular events per 38.7-mg/dL reduction in LDL-C was 0.79 (95% CI, 0.70-0.88)
statins and nonstatins combined, the RR was 0.79 (95% CI, 0.71-0.87; P < .001)
diving deeper:
defining Major Vascular Events
- nonfatal MI
- stroke
- revascularization
and the effect data
3/4 were statistically significant
the Fourier trial failed to show statistical significance.
Absolute risk reduction is marginal:
- CTTC 0.5% per annum
- IMPROVE-IT 0.4% per annum
- Fourier 1.2% per annum (invalid)
- REVEAL 0.2% per annum
- Overall – 0.46% per annum
rounding to 0.5% absolute decreased risk of MVE per year for a 38 mg/dL reduction in LDL-C.
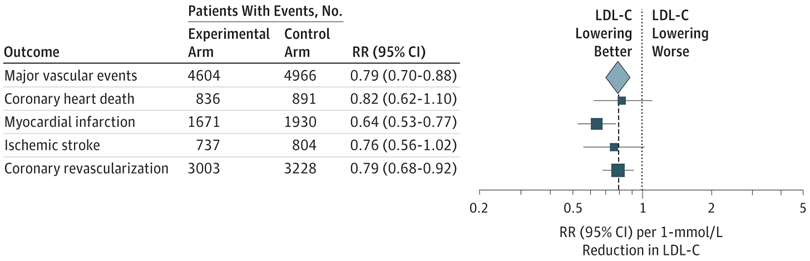
Coronary heart death was not significant
Ischemic stroke was not significant
despite being able to improve rates of MI cholesterol medication seems unable to impact CV Mortality.
In order to even achieve the prerequisite drops in LDL-C advocated for in high-risk patients evolocumab is likely necessary.
the re-analysis of the Fourier trial sparks concern for elevated CVD risk in the treatment group, lack of efficacy, and a medication that was approved for its ability to lower LDL-C and not its actual effectiveness as a medication beyond numbers on the computer screen. FOURIER showed numerically higher CV death, death from any cause despite its apparent ability to lower MI and stroke.

The lipoprotein hypothesis of heart disease I believe has fundamental flaws in the approach to treatment.
whilst oxidized pathological LDL-C is implicated in the subintimal plaque deposition on histological autopsy itappears to me that this happens at any non-zero LDL level and is not the reductionist ‘area under the curve’ argument.
References:
Sabatine MS, Wiviott SD, Im K, Murphy SA, Giugliano RP. Efficacy and Safety of Further Lowering of Low-Density Lipoprotein Cholesterol in Patients Starting With Very Low Levels: A Meta-analysis. JAMA Cardiol. 2018;3(9):823–828. doi:10.1001/jamacardio.2018.2258
https://www.nejm.org/doi/full/10.1056/NEJMoa1615664
